
Please note also that the ABA Medical Necessity Guide may be updated and are, therefore, subject to change. Some plans exclude coverage for services or supplies that Aetna considers medically necessary. The member's benefit plan determines coverage. The conclusion that a particular service or supply is medically necessary does not constitute a representation or warranty that this service or supply is covered (i.e., will be paid for by Aetna) for a particular member. Members and their providers will need to consult the member's benefit plan to determine if there are any exclusions or other benefit limitations applicable to this service or supply. Members should discuss any matters related to their coverage or condition with their treating provider.Įach benefit plan defines which services are covered, which are excluded, and which are subject to dollar caps or other limits. Treating providers are solely responsible for medical advice and treatment of members. The ABA Medical Necessity Guide does not constitute medical advice. The Applied Behavior Analysis (ABA) Medical Necessity Guide helps determine appropriate (medically necessary) levels and types of care for patients in need of evaluation and treatment for behavioral health conditions. If this is a type 1 NPI or physician/provider group, you must complete a type 1 application request form.īy clicking on “I Accept”, I acknowledge and accept that: *Do you confirm this is a type 2 facility NPI?
Questions about individual physician/provider or physician/provider groups application process? Note: A separate application needs to be submitted for each physician/provider in your group.Ĭomplete an NPI type1 individual application > Individual physicians/providers (type 1) or physician/provider groups should complete an NPI type 1 individual application. Want to contract with us? Complete this form if you are a hospital, facility, or ancillary provider only. Information about our application and credentialing process >Īs a practitioner, you have the right to correct any information obtained during the credentialing process by working directly with the reporting entities. Please ensure that your CAQH ProView or Medversant/ProviderSource™ applications are complete to avoid delays in the Credentialing process. If you need more information about our application and credentialing process, use the link below. You’ll also find information on Council for Affordable Quality Healthcare's (CAQH) ProView® and Medversant/ProviderSource™.
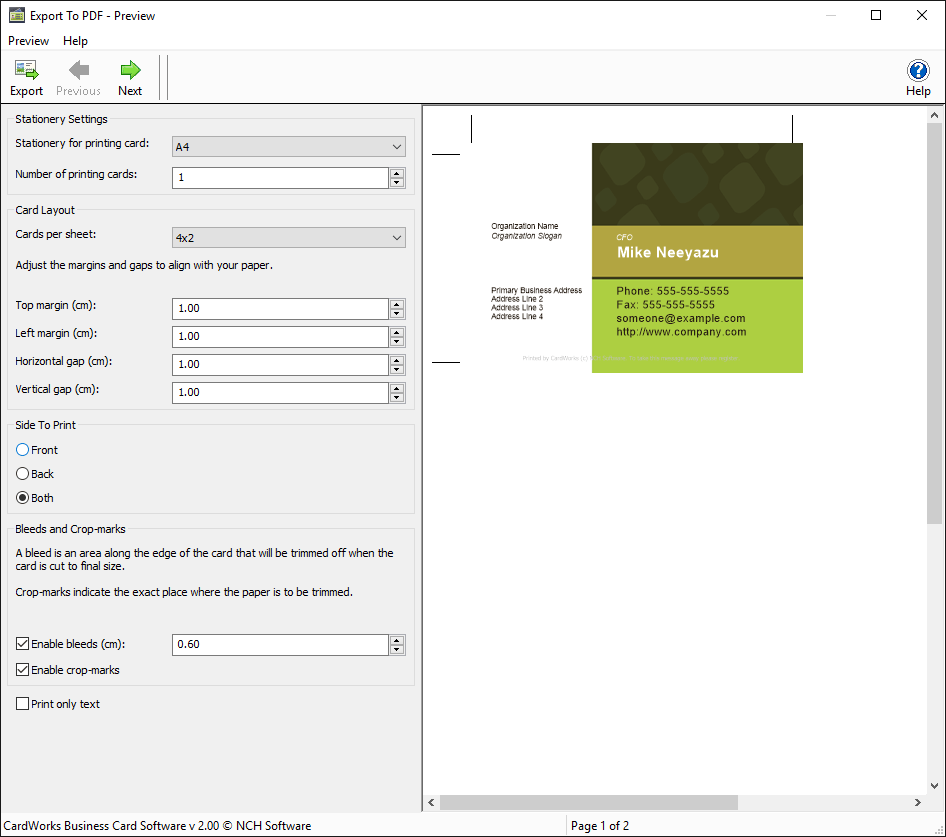
Cardworks network by aetna update#
In-Network providers can update their Tax ID by clicking on Contact and then selecting Practice changes/Provider termination from the list. If you’re already in our network, you can’t use this form to update your Tax ID.If you have multiple Tax ID’s, you only need to complete this form once for your primary service location to initiate your contracting and credentialing process.Midwife, Nurse Practitioner, Physician Assistant. Under the “specialty” question on the form, please refer to the instructions for non-physicians to select their “provider type” from the pull down menu e.g. If you are a midlevel provider complete the “medical request for participation” form.Helpful Tips to consider before completing request for participation: Please complete this form if you’re interested in joining Aetna's network and you are a medical health care professional, physician or non-physician.


 0 kommentar(er)
0 kommentar(er)
